Using Novel Recruitment Methods to Mitigate COVID-19 Spread in Marginalized Communities
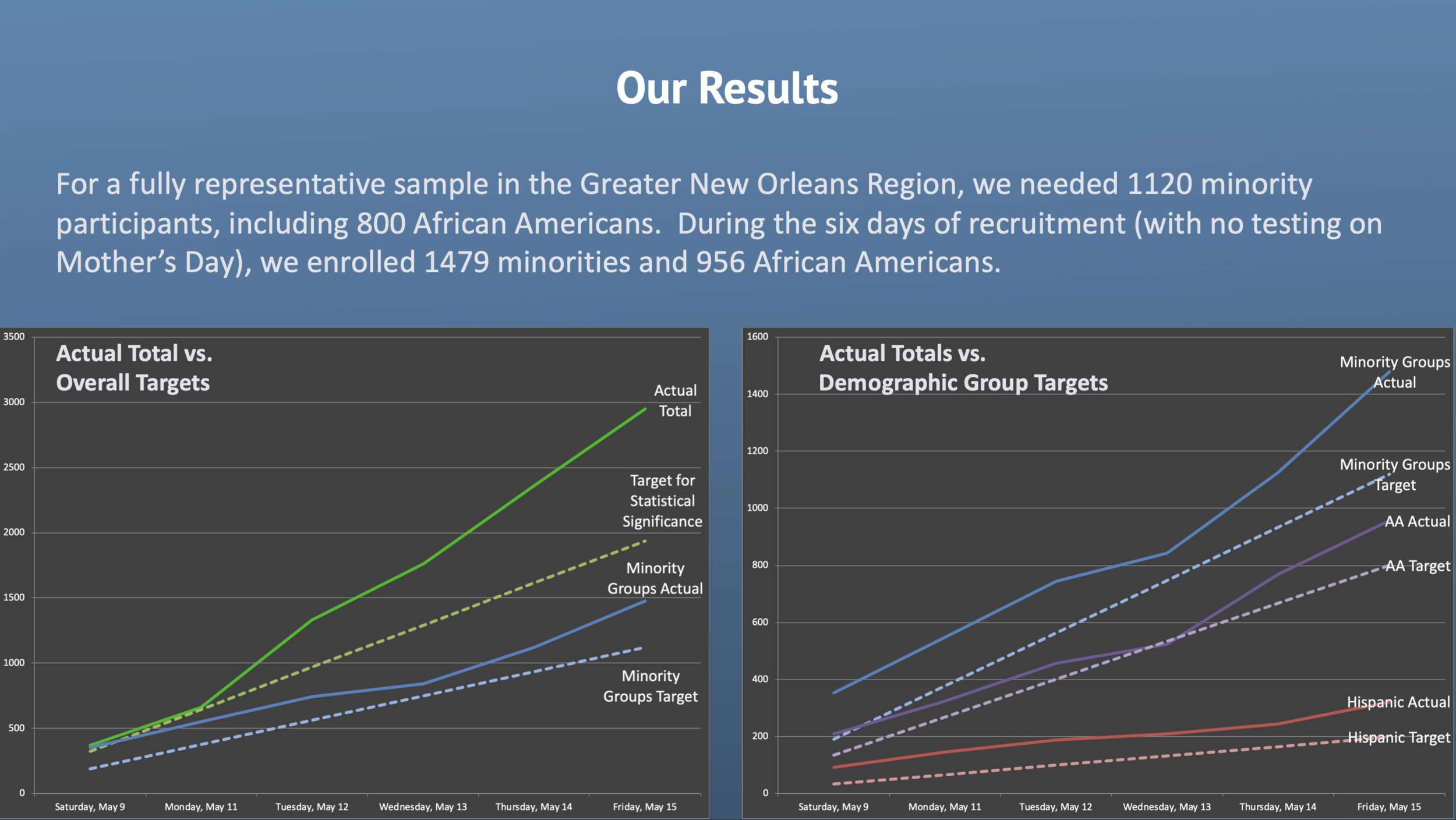
From May 9-15, Public Democracy completed the first large clinical research study to achieve a fully-representative population sample. We did this with the majority minority population of New Orleans—not by developing some new process for getting Black people to do what we wanted—but by allowing data and our empathy-based engagement tools to directly confront biases that create barriers to minority participation.


Inclusion, participation, and knowledge are essential building blocks for a Culture of Health. Yet each of these foundational elements is eroded by our current systems that permit the incomplete data sampling of minorities in public health and clinical research. Data that pays close attention to some communities’ needs, while ignoring others, causes significant damage by feeding a cycle of bias in research and medicine. These biases in data directly contribute to social determinants of health and skew public policy, philanthropy, and economic development decisions in ways that are especially harmful to communities of color but also undermine a Culture of Health for all.
But it does not have to be this way. Better data and more empathy-driven, moment-based engagement strategies can shift this paradigm. We demonstrated this in the COVID prevalence study we recruited for Ochsner Health in New Orleans. The process we used to create opportunities for these communities to claim their agency in the research process are detailed in the slides above, and some of the early break-through findings that came from this first fully representative sample are detailed in the study’s preprints below.
OUR TOOLS
We continue to focus all resources at Public Democracy toward refining and improve these tools, which allow us to:
Create on-going real-time reporting about COVID-19 at the local level;
Develop tools that enable underserved communities to claim agency in their own health choices and more fully participate and be counted in our broader public health response;
Enable more accurate assessment of COVID-19 rates as most Americans remain untested;
Build epidemiological data on COVID-19 spread to enable better historical analysis and supplement under-reported rates based on individual testing alone;
Most significantly, allow for customizable, moment-based and need-based direct digital communication with different population groups, which will become increasingly vital to ensuring accurate public health communication and triage of treatment.
Importantly, our tools operate in a PII/PHI-free environment. Instead of tracking people, our system relies on patterns of behavior to identify risk and need.
We are seeking partnerships to enable Public Democracy to support public officials in addressing this outbreak. To learn more about our process, findings, and direct applications of these tools to the current crisis, please read our white paper or contact us and put “COVID-19” in the subject line.

